Diabetes & Diabetic Retinopathy
Recently, blindness caused by diabetes has decreased significantly, thanks to the NHS Diabetic Eye Screening Programme, which was introduced by the UK National Screening Committee back in 2003. Early detection and treatment can help avoid the progression of the disease and avoid blindness. Even so, diabetic retinopathy is still a leading cause of blindness in adults in the UK, especially for those who do not get early detection.
Understanding the Disease
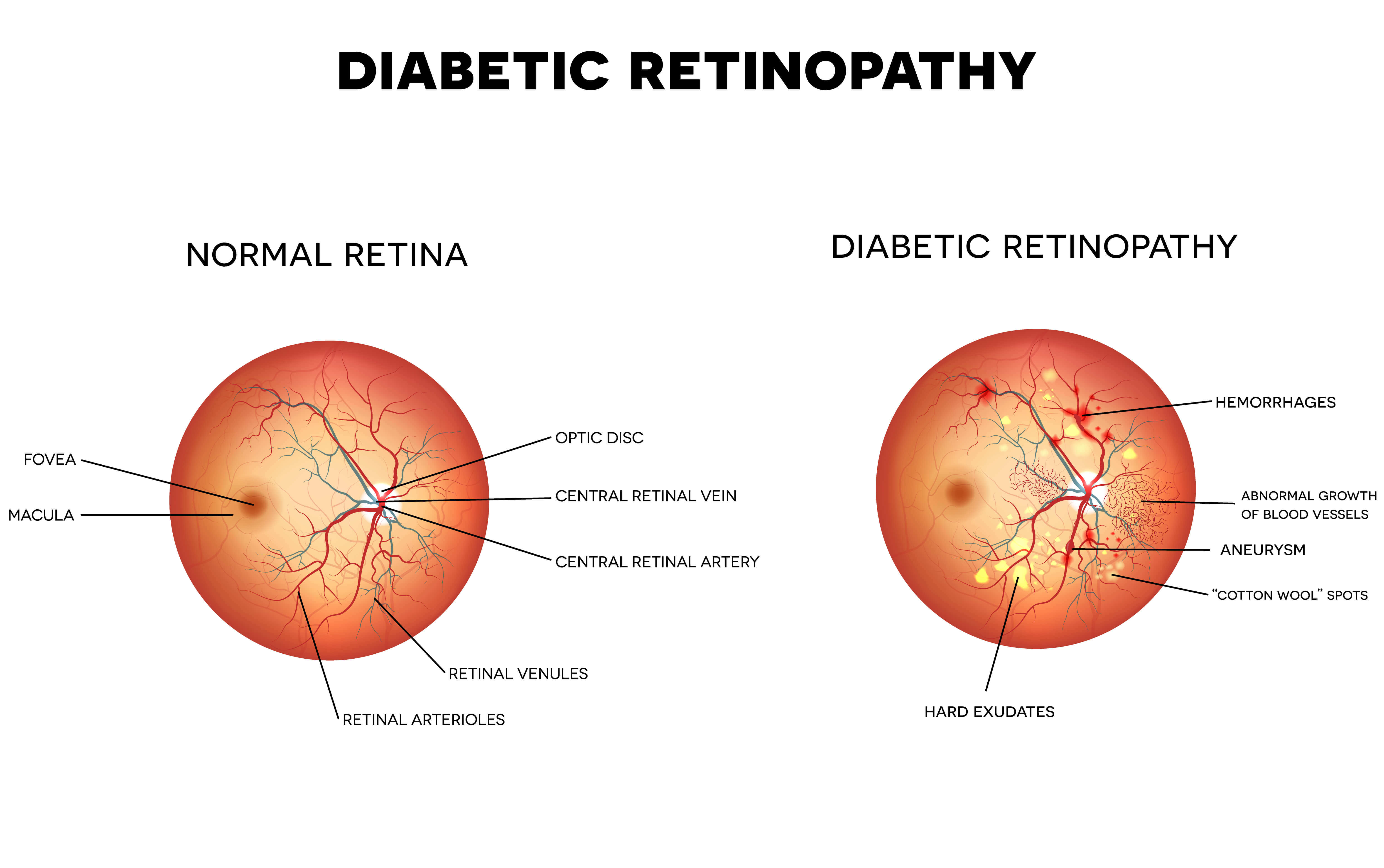
In the back of your eye is the retina. This sensitive tissue is responsible for gathering the light that passes through your cornea and relaying the information gathered into the optic nerve. Diabetics often experience issues with their circulation, this can cause the microscopic capillaries and blood vessels of the retina to bleed into the eye.
In the advanced stages of the disease, the blood vessels can grow out of control, blocking vision or even causing blindness. As over half of people with diabetic retinopathy are unaware they have it, early detection and treatment are crucial to halt its progression. This disease affects people with all types of diabetes, including Type 1, Type 2, and gestational diabetes.
The Stages of Diabetic Retinopathy
The National Eye Institute breaks the stages of disease down into four distinct groups. Your optometrist or ophthalmologist will be able to advise you of where you fall within the stages.
- Mild nonproliferative. This is the first stage. Most people will have no idea the disease is present. Upon inspecting the retina with a special microscope (ophthalmoscope), your optometrist will note tiny bulges in the blood vessels of the retina. They may or may not be leaking fluid.
- Moderate nonproliferative. At this stage, the vessels that provide the retina with oxygen and nutrients may be twisted or distorted. They may begin to close off and narrow. This can also contribute to another diabetic eye disease known as Diabetic Macular Edema (DME).
- Severe nonproliferative. The blood vessels become clogged and cut off blood supply to parts of the retina. The tissue then ceases to function and dies. This causes the body to attempt to repair itself by growing new blood vessels, which will impede vision even more.
- Proliferative. At this end stage, the damage to the retina and its blood supply is severe. New vessels may grow around the retina and into the vitreous gel of your inner eye. These new structures are fragile and bleed easily, obscuring vision even more. In severe cases, this new growth can rip the retina from the back of the eye. This is called retinal detachment and will cause complete blindness in a matter of days if not surgically treated.
Prevention of Diabetic Eye Disease
There are plenty of steps you can take to lower your risk of developing diabetic retinopathy, even if you are already diabetic. Prevention of the disease hinges on three factors:
- Making good lifestyle choices
- Knowing and managing your vital numbers
- Having regular screenings
Lifestyle choices can do a lot to lower the risks of developing the disease as well as stop the progression of the disease if you've already been diagnosed. Recent thinking is changing on the cause of Type 2 diabetes and how to control it. Doctors have always concentrated on Blood sugar levels and on long-term H1C as good indicators of whether diabetes is under control or not. However, recent studies show that the outcome of Type 2 diabetes (diabetic retinopathy, heart disease, peripheral neuropathy, kidney disease, etc) is unaltered in those patients with very strict blood sugar control, compared to those with much weaker control. The argument is that high levels of glucose are in all the body's cells, not just in the blood, and increasing insulin levels using a variety of medication simply pushes the glucose from the blood back into the cells (primarily the liver), thus masking the problem. Higher insulin levels cause insulin resistance, requiring more insulin, creating a feedback loop.
Type 2 Diabetics must understand this point: it is HIGH INSULIN levels that cause hyperglycemia and then INSULIN RESISTANCE. The conventional 'cure' is increasing medication to treat the symptoms (high blood sugars).
However, a diet very low in carbohydrates (no/very little flour products i.e bread/cakes etc), low in sugars (especially the artificially created high fructose corn syrup (which stimulates a very high insulin response), avoiding artificial sweeteners (another high insulin response), and stopping snacking can have a significant effect on reducing insulin levels, and reverse diabetes. Throw in Intermittent fasting, and you can be on your way to reversing type 2 diabetes.
If you are currently overweight or obese, resolve to lose the extra pounds right away, by using the methods discussed - especially lose belly fat. There are many prescription medications on the market to help diabetics control their eating and their weight, check out diabetes.org.uk for detailed information about what's available, and speak with your family doctor if you think they could help you.
If you smoke cigarettes, make a concerted effort to quit. Your doctor can help you with smoking cessation aids and programs. Get plenty of exercise that raises your heartbeat and gets your blood pumping. Hiking, bicycling and swimming are all excellent low-impact options. If you drink alcohol, limit yourself to no more than 14 units per week. Red wine is OK in moderation, as is dark chocolate. Avoid recreational drugs and risky behaviours that may compromise your overall health in any way.
Regular screening is also paramount. The sooner you are diagnosed and properly treated, the less of a foothold the disease will have on your retinas. You can be screened by your optometrist on a yearly basis, whenever or not it's time to update your vision correction prescription. If you don't wear glasses or contact lenses, you will need to begin seeing an optometrist for a yearly checkup as soon as you are diagnosed with diabetes. All diabetics of every age must be screened, as retinopathy can develop in young people just as easily as in older people. If your child has been diagnosed with diabetes, they will need to be seen by an optometrist right away.
Treatment of Diabetic Retinopathy
If you are within the first three stages of the disease, the best treatment possible is careful management of your blood sugar levels. If your diabetes is well-controlled, your risk of developing diabetic retinopathy decreases dramatically. All of the same steps used to prevent retinopathy, such as healthy lifestyle choices and regular screenings, are also used to treat the disease in its earlier stages.
For those who have progressed to the proliferative stage of the disease, various treatment options are available to curtail the excess blood vessel growth. This can sometimes restore lost sight, provided the retina is still attached and is receiving a blood supply. Options include:
- Laser Treatments. A laser can sometimes be used to treat the overgrowth of blood vessels obscuring the retina. Whether or not you qualify for laser treatments depends largely on the severity of the disease, with those in the first three stages usually being better candidates than those with advanced disease.
- Steroid Injections. By injecting steroids in the vitreous gel inside the eye, the pressure can be reduced. This will help reduce inflammation and allow the blood vessels in the eye to heal.
- Surgical Intervention. Surgery can be used to clear away blood that has leaked into the vitreous gel or is obscuring the retina. Surgery can also be used to remove scar tissue if laser treatment is unsuccessful or the retinopathy has advanced too far for it to be effective. Surgery is often the last resort after all other options have been exhausted.
If you are diabetic and are concerned about the possibility of diabetic retinopathy, or you have already been diagnosed, understanding the disease, prevention and treatments is integral to your health. Diabetic retinopathy usually responds well to treatment and changes in lifestyle, meaning you can control the progression and outcome.
If you have additional questions or are concerned you may be at risk, contact your optometrist, ophthalmologist, or general practitioner right away. Early detection is crucial to preserving the health of your eyes.